Components of Health Status Assessment
The primary objectives of physiological monitoring are to

Physiological monitoring, also known as biometric monitoring or biosensing, is a vital aspect of healthcare, sports science, and various other fields. It involves the continuous or periodic measurement of physiological parameters to assess an individual’s health status, performance, or response to interventions. These parameters encompass a wide range of bodily functions, including but not limited to heart rate, blood pressure, respiratory rate, body temperature, oxygen saturation, and activity level.
The primary objectives of physiological monitoring are to:
Assess Health Status:
Physiological monitoring allows healthcare professionals to track vital signs and other physiological parameters to assess a patient’s overall health and detect any abnormalities or deviations from normal values. By continuously monitoring parameters such as heart rate, blood pressure, and oxygen saturation, clinicians can identify signs of cardiovascular or respiratory distress, monitor the progress of critical illnesses, and intervene promptly when necessary.
Assessing health status is a fundamental aspect of healthcare that involves evaluating an individual’s overall physical, mental, and emotional well-being. It encompasses a comprehensive examination of various factors, including medical history, symptoms, vital signs, laboratory tests, and diagnostic imaging, to gain insight into a person’s current health condition and identify any potential issues or risks. The assessment of health status serves as the foundation for making informed decisions regarding prevention, diagnosis, treatment, and management of health conditions.
Components of Health Status Assessment:
Medical History:
Gathering a detailed medical history is the cornerstone of assessing health status. This includes information about past illnesses, surgeries, medications, allergies, family medical history, lifestyle factors, and psychosocial factors. Understanding a person’s medical history provides valuable context for interpreting current symptoms and identifying risk factors for certain diseases.
Symptom Evaluation:
Assessing symptoms involves obtaining a thorough description of any physical discomfort, pain, or changes in bodily functions that the individual may be experiencing. Symptoms can vary widely depending on the underlying cause and may include pain, fatigue, shortness of breath, dizziness, nausea, fever, cough, and changes in appetite or sleep patterns. Evaluating symptoms helps healthcare providers narrow down potential diagnoses and develop targeted treatment plans.
Vital Signs Measurement:
Vital signs, including heart rate, blood pressure, respiratory rate, and body temperature, provide essential indicators of physiological function and overall health. Monitoring vital signs allows healthcare providers to detect abnormalities or deviations from normal values that may indicate underlying health problems, such as hypertension, tachycardia, or fever. Vital signs are routinely measured during physical examinations and serve as objective measures of a person’s health status.
Physical Examination:
A thorough physical examination involves assessing various body systems, including the cardiovascular, respiratory, gastrointestinal, musculoskeletal, neurological, and integumentary systems. During the physical exam, healthcare providers may inspect the body for abnormalities, palpate for tenderness or masses, auscultate for abnormal sounds, and perform specialized maneuvers to assess function and mobility. Physical examination findings help clinicians identify signs of illness or injury and guide further diagnostic evaluation.
Laboratory Tests:
Laboratory tests, such as blood tests, urine tests, and imaging studies, provide objective data about the body’s internal functioning and help diagnose and monitor various medical conditions. Blood tests can measure levels of blood cells, electrolytes, hormones, enzymes, and other substances, while urine tests can detect abnormalities in kidney function, glucose metabolism, or urinary tract infections. Imaging studies, such as X-rays, CT scans, MRI scans, and ultrasound, allow visualization of internal structures and organs to assess for abnormalities or pathology.
Health Behavior Assessment:
Assessing health behaviors, such as diet, exercise, smoking, alcohol consumption, and substance use, is crucial for understanding an individual’s lifestyle and identifying modifiable risk factors for chronic diseases. Health behavior assessment involves gathering information about dietary habits, physical activity levels, sleep patterns, stress management techniques, and adherence to preventive health practices. Counseling and interventions aimed at promoting healthy behaviors can help improve health outcomes and prevent disease.
Importance of Assessing Health Status:
Early Detection and Prevention:
Assessing health status enables early detection of health problems and implementation of preventive measures to mitigate risks and promote optimal health. Regular health screenings and check-ups allow healthcare providers to identify risk factors and recommend appropriate interventions, such as lifestyle modifications, vaccinations, or preventive medications, to prevent or delay the onset of diseases.
Diagnostic Accuracy:
Accurate assessment of health status is essential for making accurate diagnoses and developing effective treatment plans. Gathering comprehensive information about a person’s medical history, symptoms, and physical examination findings helps healthcare providers narrow down potential differential diagnoses and order appropriate diagnostic tests to confirm or rule out suspected conditions.
Treatment Planning and Management:
Assessing health status guides the development of individualized treatment plans tailored to each person’s unique needs and preferences. Based on the assessment findings, healthcare providers can recommend pharmacological interventions, surgical procedures, lifestyle modifications, or behavioral therapies to address underlying health issues and optimize health outcomes.
Monitoring Progress:
Regular assessment of health status allows for ongoing monitoring of treatment effectiveness and disease progression. By tracking changes in symptoms, vital signs, laboratory values, and imaging findings over time, healthcare providers can evaluate the response to treatment, adjust medication doses or treatment regimens as needed, and identify any complications or adverse effects early on.
Patient Empowerment:
Empowering individuals to actively participate in their own healthcare is a key component of assessing health status. By engaging patients in discussions about their health concerns, educating them about their conditions, and involving them in shared decision-making processes, healthcare providers can promote self-management skills, adherence to treatment plans, and overall health literacy.
In summary,
Assessing health status is a multifaceted process that involves gathering comprehensive information about a person’s medical history, symptoms, vital signs, physical examination findings, laboratory tests, and health behaviors. By systematically evaluating these factors, healthcare providers can gain insight into an individual’s current health condition, identify risk factors for disease, and develop personalized strategies for prevention, diagnosis, treatment, and management of health conditions. Regular assessment of health status is essential for promoting optimal health outcomes, enhancing patient well-being, and preventing or managing chronic diseases effectively.
Diagnose and Manage Medical Conditions:
Physiological monitoring is instrumental in the diagnosis and management of various medical conditions. For example, continuous glucose monitoring is essential for individuals with diabetes to monitor their blood sugar levels and adjust insulin therapy accordingly. Similarly, ambulatory electrocardiography (ECG) monitoring helps diagnose cardiac arrhythmias and assess the effectiveness of antiarrhythmic medications or interventions.
Diagnosing and managing medical conditions is a complex and dynamic process that involves the identification, evaluation, and treatment of diseases or disorders affecting the human body. From common ailments to rare and complex conditions, healthcare professionals employ a variety of tools and strategies to accurately diagnose and effectively manage medical conditions, with the ultimate goal of improving patient outcomes and quality of life.
Diagnosis of Medical Conditions:
Clinical Assessment:
The diagnostic process often begins with a thorough clinical assessment, which includes gathering information about the patient’s medical history, symptoms, and physical examination findings. A detailed history can provide valuable clues about the onset, duration, severity, and progression of symptoms, as well as any relevant risk factors or predisposing conditions. Physical examination findings, such as abnormalities in vital signs, organ function, or specific body systems, further aid in narrowing down potential diagnoses.
Diagnostic Tests:
Diagnostic tests play a crucial role in confirming or ruling out suspected medical conditions. These tests may include laboratory tests, imaging studies, biopsies, genetic testing, and specialized procedures. Laboratory tests, such as blood tests, urine tests, and tissue biopsies, can detect abnormalities in blood cell counts, biochemical markers, hormone levels, or genetic mutations indicative of specific diseases. Imaging studies, such as X-rays, CT scans, MRI scans, and ultrasound, allow visualization of internal structures and organs to assess for structural abnormalities, tumors, or injuries.
Diagnostic Criteria and Guidelines:
Many medical conditions have established diagnostic criteria and guidelines based on evidence-based medicine and expert consensus. These criteria outline specific clinical features, laboratory findings, imaging characteristics, and other parameters necessary for making a definitive diagnosis. Healthcare professionals rely on these criteria to standardize the diagnostic process, ensure accuracy and consistency in diagnosis, and facilitate appropriate management and treatment decisions.
Multidisciplinary Approach:
Diagnosing complex or rare medical conditions often requires a multidisciplinary approach involving collaboration among healthcare professionals from different specialties. Multidisciplinary teams may include physicians, surgeons, radiologists, pathologists, geneticists, and other specialists who contribute their expertise and knowledge to arrive at an accurate diagnosis and develop a comprehensive treatment plan.
Management of Medical Conditions:
Pharmacological Interventions:
Pharmacological interventions, including medications and drugs, are commonly used to manage medical conditions by alleviating symptoms, controlling disease progression, and improving overall health outcomes. Medications may include antibiotics for bacterial infections, analgesics for pain relief, anti-inflammatory drugs for inflammation, antihypertensive drugs for high blood pressure, and antidiabetic drugs for diabetes management, among others. Healthcare providers prescribe medications based on the underlying pathophysiology of the condition, individual patient factors, and considerations for efficacy, safety, and potential adverse effects.
Surgical Interventions:
Surgical interventions may be necessary to treat certain medical conditions that cannot be adequately managed with conservative measures or medications alone. Surgical procedures range from minimally invasive techniques, such as arthroscopy or laparoscopy, to more complex surgeries, such as organ transplants or tumor resections. Surgeons perform surgeries to remove diseased tissues, repair anatomical defects, restore normal function, or alleviate symptoms, with the goal of improving patient outcomes and quality of life.
Non-pharmacological Interventions:
Non-pharmacological interventions, such as lifestyle modifications, physical therapy, occupational therapy, dietary changes, and psychotherapy, play an important role in managing many medical conditions. These interventions aim to address underlying risk factors, improve symptoms, enhance functional abilities, and promote overall well-being. For example, lifestyle modifications, such as smoking cessation, weight management, regular exercise, and stress reduction techniques, can help prevent and manage chronic diseases like cardiovascular disease, diabetes, and hypertension.
Patient Education and Self-management:
Patient education and self-management strategies empower individuals to take an active role in managing their own health and well-being. Healthcare providers educate patients about their medical conditions, treatment options, potential complications, and strategies for self-care. Patients learn how to monitor their symptoms, adhere to medication regimens, follow dietary and lifestyle recommendations, recognize warning signs of worsening conditions, and seek appropriate medical attention when necessary. Patient education fosters collaboration between patients and healthcare providers, enhances treatment adherence, and improves health outcomes.
Long-term Monitoring and Follow-up:
Managing chronic medical conditions often requires long-term monitoring, regular follow-up appointments, and adjustments to treatment plans based on disease progression, treatment response, and changes in patient needs. Healthcare providers monitor patients’ symptoms, vital signs, laboratory values, and imaging findings over time to assess treatment efficacy, detect complications, and optimize therapeutic interventions. Regular follow-up appointments provide opportunities for patient education, medication reconciliation, preventive care, and addressing any concerns or questions that may arise.
Challenges and Considerations:
Complexity of Medical Conditions:
Many medical conditions are multifactorial and complex, making diagnosis and management challenging. Some conditions may present with nonspecific symptoms or overlap with other diseases, leading to diagnostic uncertainty and delays in treatment initiation. Healthcare providers must carefully consider differential diagnoses, conduct thorough evaluations, and collaborate with specialists to ensure accurate diagnosis and appropriate management.
Individual Variability and Personalized Medicine:
Each patient is unique, with individual characteristics, preferences, and responses to treatment. Personalized medicine emphasizes tailoring healthcare interventions to each person’s specific needs, genetic makeup, and environmental factors. Healthcare providers strive to deliver patient-centered care by considering factors such as age, gender, ethnicity, comorbidities, medication tolerance, socioeconomic status, and psychosocial support when developing treatment plans.
Cost and Resource Constraints:
The management of medical conditions may be limited by cost constraints, resource availability, and healthcare system factors. Access to diagnostic tests, medications, surgical procedures, and specialized therapies may vary depending on geographic location, insurance coverage, healthcare infrastructure, and socioeconomic disparities. Healthcare providers must balance the benefits and risks of treatment options while considering cost-effectiveness, equity, and patient preferences.
Adherence and Compliance:
Treatment adherence and patient compliance play critical roles in the successful management of medical conditions. Adherence to medication regimens, lifestyle modifications, and follow-up appointments can significantly impact treatment outcomes and disease progression. Healthcare providers employ strategies such as patient education, motivational interviewing, medication reminders, and social support networks to promote adherence and address barriers to compliance.
In conclusion,
Diagnosing and managing medical conditions require a comprehensive and multifaceted approach that integrates clinical assessment, diagnostic testing, pharmacological and non-pharmacological interventions, patient education, and long-term monitoring. Healthcare providers strive to accurately diagnose conditions, develop personalized treatment plans, and empower patients to actively participate in their own care. Despite challenges and complexities, effective management of medical conditions improves patient outcomes, enhances quality of life, and promotes overall health and well-being.
Optimize Sports Performance:
Physiological monitoring is widely used in sports science to assess athletes’ physical fitness, monitor training loads, and optimize performance. By tracking parameters such as heart rate variability, lactate threshold, and oxygen consumption, coaches and athletes can design training programs tailored to individual needs, prevent overtraining, and maximize performance during competitions.
Optimizing sports performance is a multifaceted process that involves enhancing athletic abilities, maximizing physical fitness, refining technical skills, and improving mental toughness to achieve peak athletic performance. Whether in individual or team sports, athletes and coaches employ a variety of strategies, training methods, and technologies to optimize performance and gain a competitive edge. From training regimens and nutrition plans to sports psychology and biomechanical analysis, optimizing sports performance encompasses a wide range of factors that contribute to athletic success.
Training and Conditioning:
Strength Training:
Strength training is a cornerstone of sports performance optimization, aiming to increase muscle strength, power, and endurance. Athletes perform exercises such as weightlifting, resistance training, plyometrics, and functional movements to develop muscle mass, improve explosive power, and enhance overall athletic performance.
Endurance Training:
Endurance training focuses on improving cardiovascular fitness, aerobic capacity, and stamina to sustain prolonged physical activity. Athletes engage in activities such as running, cycling, swimming, and cross-training to build endurance, increase oxygen uptake, and delay fatigue during competition.
Speed and Agility Training:
Speed and agility training are essential for sports that require quick bursts of acceleration, rapid changes in direction, and swift movements. Athletes perform drills, sprints, agility ladder exercises, and plyometric jumps to enhance speed, agility, coordination, and reaction time on the field or court.
Flexibility and Mobility Training:
Flexibility and mobility training involve stretching, yoga, mobility exercises, and foam rolling to improve joint range of motion, reduce muscle stiffness, and prevent injuries. Maintaining optimal flexibility and mobility allows athletes to move more efficiently, perform technical skills with precision, and recover faster from intense training sessions.
Skill Development:
Mastering technical skills and sport-specific techniques is crucial for optimizing sports performance. Athletes practice fundamental skills, refine their technique, and simulate game-like scenarios to enhance their proficiency and decision-making abilities under pressure.
Nutrition and Hydration:
Balanced Diet:
Proper nutrition is essential for fueling athletic performance, supporting muscle growth and repair, and optimizing recovery. Athletes consume a balanced diet rich in carbohydrates, protein, healthy fats, vitamins, and minerals to meet their energy needs, maintain optimal body composition, and enhance performance.
Hydration:
Hydration plays a critical role in athletic performance, influencing energy levels, thermoregulation, and cognitive function. Athletes maintain hydration by drinking adequate fluids before, during, and after training or competition, paying attention to electrolyte balance and individual sweat rates to prevent dehydration and heat-related illnesses.
Supplementation:
Some athletes use dietary supplements to complement their nutrition and support performance goals. Common supplements include protein powders, branched-chain amino acids (BCAAs), creatine, caffeine, and electrolyte replacements. However, athletes should exercise caution when using supplements and consult with a qualified sports nutritionist or healthcare provider to ensure safety and efficacy.
Sports Psychology:
Mental Preparation:
Mental preparation is a crucial aspect of optimizing sports performance, involving goal setting, visualization, positive self-talk, and pre-performance routines. Athletes mentally rehearse their skills, visualize success, and cultivate confidence, focus, and resilience to perform at their best under pressure.
Stress Management:
Managing stress and anxiety is essential for maintaining optimal performance and coping with competitive pressures. Athletes utilize relaxation techniques, mindfulness meditation, deep breathing exercises, and stress-reduction strategies to calm their nerves, control arousal levels, and stay composed during high-stakes situations.
Motivation and Goal Setting:
Setting clear, achievable goals and maintaining intrinsic motivation are key drivers of sports performance optimization. Athletes establish short-term and long-term goals, monitor progress, celebrate milestones, and stay committed to their training regimen and performance objectives.
Biomechanical Analysis:
Movement Analysis:
Biomechanical analysis helps optimize sports performance by evaluating movement patterns, technique, and efficiency. Motion capture systems, force plates, and 3D motion analysis software provide objective data on factors such as stride length, joint angles, ground reaction forces, and center of mass displacement, allowing athletes and coaches to identify areas for improvement and refine technique accordingly.
Equipment Optimization:
Biomechanical analysis is also used to optimize sports equipment, such as footwear, apparel, and gear, to enhance performance and reduce injury risk. By studying the biomechanics of equipment interactions with the body, researchers and manufacturers design products that improve comfort, support, stability, and aerodynamics, ultimately enhancing athletic performance.
Recovery and Regeneration:
Rest and Sleep:
Adequate rest and quality sleep are essential for recovery, muscle repair, and overall health and well-being. Athletes prioritize sleep hygiene, establish regular sleep schedules, and create conducive sleep environments to ensure optimal restorative sleep and maximize recovery between training sessions and competitions.
Nutrition and Hydration:
Proper post-exercise nutrition and hydration support recovery by replenishing glycogen stores, repairing muscle tissue, and promoting hydration and electrolyte balance. Athletes consume nutrient-rich foods and beverages containing carbohydrates, protein, and fluids within the post-workout recovery window to facilitate muscle recovery and adaptation.
Active Recovery:
Active recovery strategies, such as low-intensity exercise, swimming, cycling, or yoga, help enhance blood flow, reduce muscle soreness, and promote relaxation and recovery. Athletes engage in active recovery sessions between intense training sessions to accelerate recovery, prevent overtraining, and maintain optimal performance levels.
Recovery Modalities:
Various recovery modalities, such as massage therapy, compression garments, cold-water immersion, and contrast baths, are used to alleviate muscle fatigue, inflammation, and soreness, and facilitate recovery. Athletes incorporate these modalities into their recovery routines to accelerate muscle repair, reduce recovery time, and enhance readiness for subsequent training or competition.
Monitoring and Evaluation:
Performance Metrics:
Athletes and coaches use performance metrics and objective measures to assess progress, track improvements, and evaluate training effectiveness. Performance metrics may include time, distance, speed, power output, heart rate, and technique quality, depending on the sport and training goals.
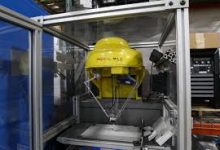
Technology and Wearables:
Advances in technology and wearables, such as GPS trackers, heart rate monitors, activity trackers, and wearable sensors, enable real-time monitoring of training loads, physiological responses, and performance metrics. Athletes use these devices to gather data, analyze trends, and make informed decisions about training adjustments, recovery strategies, and performance optimization.
Biometric Monitoring:
Biometric monitoring systems, such as heart rate variability (HRV) monitoring, provide insights into an athlete’s physiological readiness, recovery status, and adaptive capacity. By tracking changes in HRV, sleep quality, and other biometric markers over time, athletes and coaches can optimize training schedules, tailor recovery interventions, and prevent overtraining or burnout.
Feedback and Reflection:
Continuous feedback and self-reflection are integral parts of the performance optimization process. Athletes review training sessions, competitions, and performance data to identify strengths, weaknesses, and areas for improvement. Coaches provide constructive feedback, guidance, and support to help athletes refine their skills, adjust their training strategies, and achieve their performance goals.
In conclusion, optimizing sports performance requires a comprehensive and integrated approach that encompasses physical conditioning, nutrition, mental preparation, biomechanical analysis, recovery strategies, and continuous monitoring and evaluation. Athletes and coaches collaborate to
Enhance Rehabilitation and Physical Therapy:
Physiological monitoring plays a crucial role in rehabilitation and physical therapy by providing objective data to assess patients’ progress and adjust treatment plans accordingly. For example, wearable motion sensors can track movement patterns and gait parameters in individuals undergoing rehabilitation after injury or surgery, allowing therapists to monitor recovery progress and identify areas for improvement.
Monitor Sleep and Circadian Rhythms:
Physiological monitoring is used to evaluate sleep quality and monitor circadian rhythms, which play a vital role in overall health and well-being. Devices such as polysomnography systems and wearable sleep trackers measure parameters such as brain waves, eye movements, muscle activity, and heart rate variability to assess sleep stages, detect sleep disorders such as sleep apnea or insomnia, and evaluate the effectiveness of interventions such as sleep hygiene practices or medications.
Support Remote Patient Monitoring and Telehealth:
With advances in wearable sensors and wireless communication technologies, physiological monitoring has become increasingly accessible for remote patient monitoring and telehealth applications. Patients can use wearable devices or smartphone apps to track their vital signs and share real-time data with healthcare providers, enabling remote monitoring of chronic conditions, early detection of health deterioration, and timely intervention without the need for frequent clinic visits.
Technological advancements have revolutionized physiological monitoring, making it more convenient, accurate, and cost-effective. Wearable devices, such as fitness trackers, smartwatches, and medical-grade biosensors, have become ubiquitous, allowing individuals to monitor their health and fitness in real-time. These devices can track a wide range of physiological parameters, including heart rate, activity level, sleep patterns, and even electrocardiograms (ECGs) or blood glucose levels, depending on the device’s capabilities.
Furthermore, the integration of physiological monitoring with artificial intelligence (AI) and data analytics has the potential to unlock valuable insights from large-scale biometric data sets. Machine learning algorithms can analyze patterns in physiological data to identify trends, predict health outcomes, and personalize interventions based on individual characteristics and preferences.
Despite its immense potential, physiological monitoring also presents challenges and limitations. Data privacy and security concerns, interoperability issues, and the need for validation and standardization of measurement techniques are some of the challenges that need to be addressed to realize the full potential of physiological monitoring technologies.
In conclusion,
Physiological monitoring is a vital tool for assessing health status, optimizing performance, managing medical conditions, and enhancing overall well-being. With ongoing advancements in technology and data analytics, physiological monitoring has the potential to revolutionize healthcare delivery, empower individuals to take charge of their health, and improve outcomes across diverse settings and populations.